Telemedicine
Providing Care at a Distance
👉 Slides available for MCW students here
Introduction to Telemedicine
Definitions Telemedicine is clinical care provided at a distance through audio/video telecommunications systems.
Particularly in areas where access can be difficult (e.g. rural areas), telemedicine provides a way for people to receive care even with challenges of time and space/distance.
Telemedicine can be considered a subset of telehealth, which would include other provisions of care including public health practice. Terms such as virtual care or virtual health are usually synonymous with a form of telehealth, but are more commonly used in the consumer space.
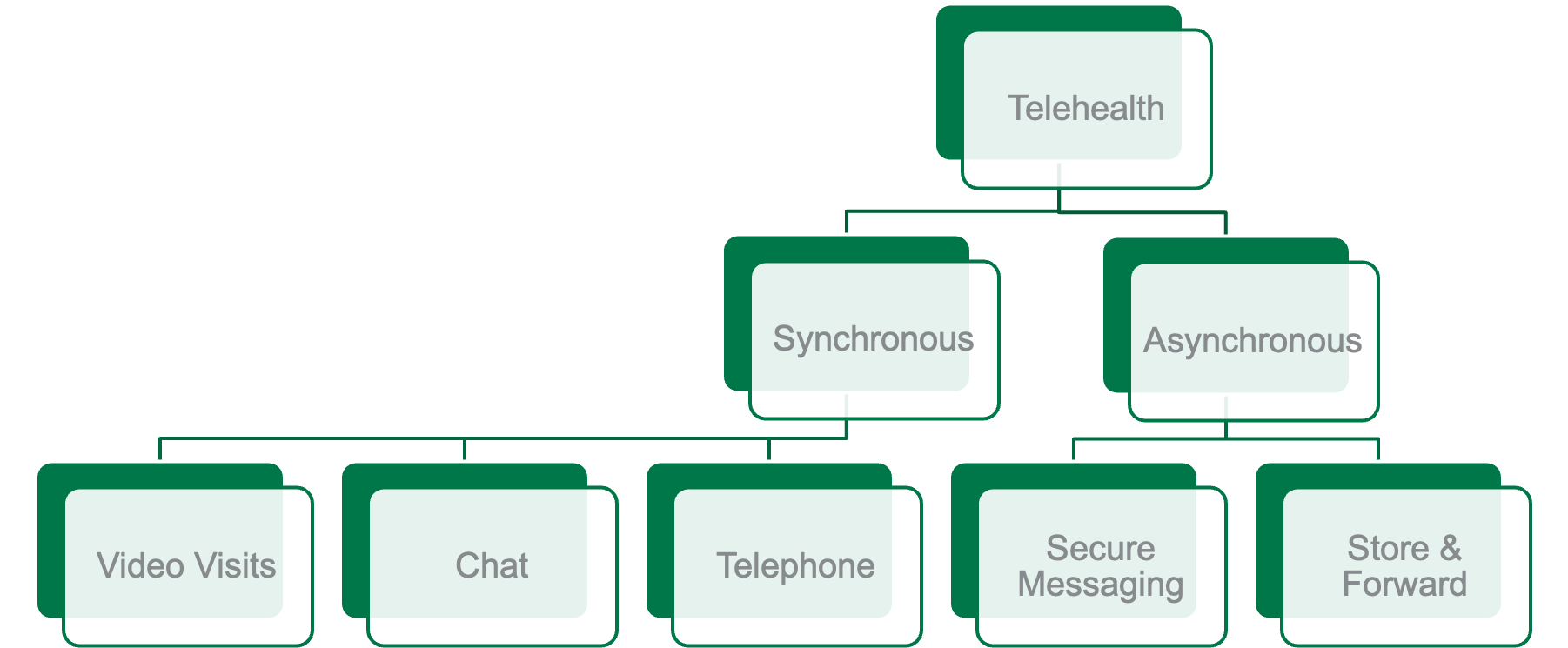
Telemedicine can be broken down into a few different modalities....
- Synchronous -- e.g. care provided in real time
- Asynchronous -- care that is usually 'store and forward' conceptually, where information is provided ahead of time by a patient or a clinician, and then reviewed later by a specialist or expert.
Telemedicine is a concept nested under telehealth, which is slightly more broad and include public health include other aspects of health care services as well. Synchronous can be video based. It could be chat, which generally now are being looked at for nurse triage lines. Even the VA hospital has a pilot where they're using chat functionalities for patients to go through triage processes, and then telephone-based care as well.
Asynchronous care include ssecure messaging, such as you might send to a clinician, as well as more encapsulated episodes of care that are called store and forward. So these might be taking a picture of a rash, and then sending it to a dermatologist. This could include tele ophthalmology were at a primary care office a patient has a retinal image taken. And those are then sent, and then at some time later, an ophthalmologist will review all of those images looking for signs of diabetic retinopathy as just one example. And they can also be asynchronous visits for common medical conditions, including urinary tract infections, back pain, or contraception.
There are several different modalities within synchronous telemedicine that we will touch on
- Hub and Spoke Model
- Direct to consumer
- Remote observation, including teleICU care
The COVID-19 pandemic that hit in earnest in 2020 accelerated several changes within helath care worldwide to accelerate telemedicine
But first, a little review of history.
A (very) Brief History of Telemedicine
The mainstream availability and usage of the telephone was a critical change that ushered in the area of care at a distance. A 1954 article in JAMA described how the telephone was changing clincial practices, both increasing access to the doctor while also creating new concerns for boundaries, technology challenges, and quality/safety. 👇
Before then, there were vangard uses of telegraph or telephone for assistance with diagnostics. A nice summary exists in the Understanding Telehealth book(Karen Schulder Rheuban, Elizabeth A. Krupinski Eds.) that references an 1879 report in the Lancet to listen to a cough for diagnosis of croup, and in 1905 for the transmission of cardiophonetics for a 'telecardiogram.'(Described in History of Telemedicine)
the case of an anxious mother who convinced that her baby had the crew, called the infant's grandma for assistance the ladder in turn telephone the family doctor at midnight and told them the terrible news. Perhaps because of the lateness of the hour and the doctor asked to be put in telephonic communication with the anxious Mama. "Lift the child to the telephone he commanded." And let me hear it cough. Both mother and child complied. That's not the croup the doctor declared and declines to leave his house on such small matters and advised grandma also to stay in bed...all anxiety quieted. The trio settle down happily for the night. I don't know if that was the best bedside manner... but this was an actual report of a physical examination remotely for the purpose of diagnosis and triage.
System Components
Video conferencing systems including technology, internet connectivity, and transmitting and receiving technologies. These can include robust specific hardware/software combinations for telepresence as well as consumer or professional software suites e.g. Cisco, Zoom.
Camera equipment can include simple web cameras to more involved telepresence systems. We have found that tablet or smartphone integrated cameras can be very useful and effective.
Ancillary Diagnostic Tools including tools for remote otoscopy, auscultation, or visualization. For example, tools can take live images from diagnostic scopes. Heart and lung sounds can be transmitted (or stored for subsequent download) for review by remote clinicians. Remote vital signs and ECGs may also be transmitted. Special lenses or adapters may also be used to take images with additional detail, such as for dermatologist review.
Image Transmission Images may be stored and forwarded to later locations. These may include images within a Picture Archiving and Communications System(PACS).
Care Models
Hub and Spoke
The Hub and Spoke model for telemedicine considers the specialist or treating physician to be in a central location, and the spokes to be remote distance sites. Spoke sites are traditionally clinics that have high-speed connectivity and dedicated video conferencing technology. Spoke sites may also be spaces within pharmacies, kiosks, and now even homes.
Clinicians and/or patients may be at the spoke. An example of a patient/clinicain to specialist consultation is in telestroke. There, a neurologist may observe the physical exam, review imaging, and provide guidance to the on-site treating physician.
An example of a clinican to clinician consultation is Project Echo, where spoke sites meet regularly with centralized expertise in a hub site to review cases, provide education, and assist with patients with challenging conditions or presentations. Project Echo was first conducted in New Mexico as a way to assist primary care physicians in treating hepatitis C with newer medications. There were simply not enough hepatolgoists or infectious disease physicians distributed across the state where the needs were high. But at the University of New Mexico, S. Arora and colleagues provided education and guidance, resulting in many more people being successfulyl treated for hepatitis C.
Direct to Consumer
Increasingly, and especially during COVID-19, direct to consumer telemedicine became very popular. In the mid-2010s, more companies began offering direct to consumer telemedicine services. Many of these were focused on urgent care, and lower acuity medical conditions. Mental health services, in particular, we're very representative of the changes and services that were being seen. Many insurance companies begin offering such services as well as to meet their members needs, while keeping costs relatively low. Companies, such as American well, began offering such services, and all develop the market for physicians who wanted to work part time doing virtual on-demand care, similar to other industries that have seen people take part time shifts for work.
Healthcare systems they can also offering a direct to consumer services. Somewhere for primary care, both longitudinal and episodic/urgent care, and others outsource these to Other on demand care offerings.
Historically, many insurance companies, particularly Medicare, did not cover for virtual care services that were direct to consumer, requiring patients seeking such services to be in a previously to find hub and spoke model, where the spoke was generally another clinical office, and there were certain limitations or restrictions on services, such that the patient need to be in a rural service area. During the COVID-19 pandemic, many of these barriers were lifted. In August 2020 executive order made clear that many of these changes were to be made permanent.
Tele-ICU care
The remote monitoring of intensive care patients is termed remote ICU or e-ICU. Remote vital signs may be monitored and nurses may receive support from remote critical care nurses or intensive care physicians.
Aerospace Medicine
NASA has pioneered telemedicine remote patient monitoring for astronauts in its programs.
Safety and Quality
Safety and qualty are core areas of concern as they relate to telemedicine. Can clinicians properly diagnose patients without in-person care and a full physical examination? Are the direct to consumer telemedicine providers engaging in inappropriate prescribing? For the most part, these large concerns can be allayed by data to date. During the COVID-19 pandemic, our internal data show that nearly all patients rated that they agreed or strongly agreed that their health care needs were met by telemedicine.
What about rates of antibiotic prescribibg? Shi et al provided an analysis that looked at claims data from a commercial insurer that provided telehealth services and claims for in-person PCP and urgent care. They matched telemedicine users with people who went to the PCP and went to urgent care. In general antibiotic use was actually more guideline-concordant for conditions where antibiotics were probably indicated. The caveat is that more broad spectrum antibiotics were used (lack of access to strep tests?) and follow-up visits were more frequent in the telemedicine group than the in-person care group. Antibiotics were slightly more prescribed, however, for conditions like bronchitis where antibiotics are rarely indicated.
See
- Shi Z, Mehrotra A, Gidengil C, Poon SJ, Uscher-Pines L, and Ray KN. 12/2018. “Quality of care for acute respiratory infections during direct-to-consumer telemedicine visits for adults.” Health Affairs , 37, 12, Pp. 2014-2023.
- Ray KN, Shi Z, Gidengil CA, Poon SJ, Uscher-Pines L, and Mehrotra A. 2019. “Antibiotic Prescribing During Pediatric Direct-to-Consumer Telemedicine Visits.” Pediatrics , 143, 5, Pp. e20190631
Health Policy and Reimbursement
The concerns around telemedicine were that it would create "supply induced demand, meaning that the friction that was inherent to seeking care (co-pays, driving to offices) was helpful to controlling costs -- at least from an insurance perspective. Unfortunately this policy perspective puts the burden on patients and families to determine when they should seek care, which could potentially be very costly such as an emergency department visit.
The hub and spoke model has been written into legislation, namely the Social Security Act, requiring only valid originating sites be eligible for payment. Generally these are in rural health professions shortage areas, and they are not included in urban areas or within a Metropolitan Statistical Area (MSA). These sites may include:
- physician offices
- critical access hospitals
- clinics,
- Federally qualified health centers
- hospitals
- skilled nursing facilities
- dialysis facilities.
Legislation passed at the beginning of COVID provided waivers for the originating site provision.
Costs of Telemedicine
It was this concept of how much should telemedicine cost? Should it be less expensive than in-person care? Should it be reimbursed less, accordingly, or should it be reimbursed the same? Some states have required payment parity for telehealth.
| Telemedicine | In-Person Care |
|---|---|
| Staff to support virtual rooming | Staff to support rooming |
| Technology platforms, computing systems, and networking | Examination Room Space |
| Electronic Health Record | Electronic Health Record |
| Electricity for information systems | Electricity / Heat |
| Clinician Time | Clinician Time |
| Insurance (malpractice, cyberinsurance) | Insurance (malpractice) |
An analysis done by Ashwood and colleagues looked at patients in commercial insurance system. They looked at their access to telemedicine. And so, the hypothesis was if telemedicine is going to decrease costs, say from an insurance perspective, at least, or a payer perspective, that if you had more tele health visits, you would offset those through less in person visits. But they saw that overall, even with telehealth, visit volumes for in person care increased. They increased marginally less than those without telemedicine, but overall the telehealth visits added rather than subtracted costs to the system.. on average $45/telehealth user. So their conclusion is, it may may care more convenient, but it may increase your overall spending for healthcare services.
See also
- Barnett Ml, Ray KN, Souza J, and Mehrotra A. 11/27/2018. “Trends in Telemedicine Use in a Large Commercially Insured Population, 2005-2017.” JAMA Internal Medicine , 320, 20, Pp. 2147-2149.
Access and Equity
In direct to consumer telemedicine, there is potential to worsen health care disparities. Two 2020 articles published in JAMA Internal Medicine added to what we know about this topic. The first looked at telemedicine unreadiness among older adults -- how well equipped are you to have a telemedicine visit? In their analysis, up to 38% (13 million) 65 and older have someone readiness for telemedicine, and even 20% or have unreadiness for the telephone. And that can be somewhat helped by social support, but means that more isolated people are at a notable disadvantage.
The second looked at digital access. Over a quarter of Medicare beneficiaries in 2018 had no digital access, meaning they couldn't have a video visit. This was clearly not distributed equally among racial and social economic groups.
see
- Lam K, Lu AD, Shi Y, Covinsky KE. Assessing Telemedicine Unreadiness Among Older Adults in the United States During the COVID-19 Pandemic. JAMA Intern Med. 2020. doi:10.1001/jamainternmed.2020.2671
- Roberts ET, Mehrotra A. Assessment of Disparities in Digital Access Among Medicare Beneficiaries and Implications for Telemedicine. JAMA Intern Med. 2020;180: 1386–1389
And then there is broadband access and connectivity. Data published has shown that in rural counties especially, broadband penetration is associated with accessing and using telehealth services. This highlights the role of governmental programs and/or private-public partnerships for expanding internet access into rural communities, such as through FCC initiatves.
But even among urban areas, access is not distributed equally. Analysis that we have done has identified areas of 'cold spots' in video visit adoption in urban Milwaukee communities.
See
- Wilcock AD, Rose S, Busch AB, Huskamp HA, Uscher-Pines L, Landon B, and Mehrotra A. In Press. “Is broadband internet a barrier to telemedicine use?” JAMA Internal Medicine